by Ivo Tarfusser, MD
Updated: 2019-10-20
When searching information about endoscopic thoracic sympathectomy (ETS) or related surgeries on the web or in the scientific literature, it is easy to get confused in the jungle of controversial statements, comments and claims from medical professionals, patients, communities, etc. There has been some effort to standardize certain issues, like the evaluation of quality of life parameters, but there is still too much vagueness when defining details of methods, procedures and outcomes, which makes it almost impossible, not only for patients but also for surgeons, to evaluate and compare methods and results of ETS surgery. This methodological chaos was already mentioned in D. Kopelman and M. Hashmonai's analysis from 2008 ("The Correlation Between the Method of Sympathetic Ablation for Palmar Hyperhidrosis and the Occurrence of Compensatory Hyperhidrosis", World Journal of Surgery, 11/2008, Volume 32, Issue 11).
Judgements on ETS range from miracle cure, with really remarkable results, to anger, regret and condemnation of this surgery. In some countries, the use of ETS has been limited or even prohibited, after a number of patients had suffered or serious complications. For most patients, ETS has represented a significant improvement of their quality of life, but there is a minority of patients who struggle with severe long-term side effects. It is highly likely that this divergence has to be attributed to factors related to the surgical technique, rather than to the patient's individual predisposition for adverse reactions to correctly performed ETS surgery.
In fact, for the layman (the patient), and not only, it may be astonishing to detect that there are so many different ways to perform ETS surgery. And that there is still an incredible chaos regarding the terminology (e.g. ETS T3, T2, T2+T3, T4, R2, R3, etc.). Even more surprising is that correctly performed procedures (and there are only few of them), observing the principle of minimal trauma at the best level to reach a good result, are reported with the same identical label (e.g. ETS T3) in the literature, as techniques that euphemistically can be described as far from optimum. The latter are with little doubt responsible for many unfavorable outcomes of ETS. Needless to say that this makes it difficult or impossible to evaluate and compare any of the short- and long-term results reported in the majority of the published articles.
Since my fellow colleagues Göran Claes and Christer Drott started pioneering ETS surgery in the late -80ies in Borås, Sweden, the author has been following and performing sympathetic surgery for, carrying out 3500+ ETS procedures in over 1800 patients.
During the first years, the commonly employed technique was a rib-oriented R2-3-4 sympathicotomy (imprecisely called ETS "T2-4"), using blend-mode electrocautery, later revised to R2-3 sympathicotomy (ETS "T2-3").
In the early years, slight to moderate side-effects (especially compensatory sweating) were reported by many patients and considered to be a tollerable and acceptable trade-off to get rid of debilitating focal hyperhidrosis. Severe unfavorable side-effects, particularly compensatory hyperhidrosis and, in rare cases, critical bradycardia, did not become immediately apparent. In the 1990-ies with increasing numbers of surgeries, however, detrimental side-effects turned gradually out to be a potential sequel of ETS in a minority of patients.
As a consequence, the author has ever since focused on analysing critically the technical details of ETS, trying to detect and understand the possible factors responsible for untoward side-effects. Over the years, in my surgical approach, technical changes were sequentially implemented, step by step, in order to correct procedural details that had been identified as potential causes for less favorable outcome. Additional knowledge regarding methodological shortcomings had been gained when re-operating patients, originally operated in other units, in whom the result had not turned out as expected. Modifications that appeared to improve the immediate and, most of all, the long-term clinical result were implemented into the author's surgical routine. Often the improvement was so obvious that a controlled verification study could not be carried out, as it would have required to persevere with methods that had proven inferior or even harmful.
This article, therefore, represents a wrap-up of this personal experience and is meant as a critical overview of available methods. It is not based on orthodox evidence based studies or reviews of published studies. It should try to unravel the incredible confusion that reigns in this particular field of surgery and may contribute to shed some light on why there is such degree of uncertainty and difficulty to compare the results of ETS.
In most cases, identifying and interrupting the sympathetic chain is a relatively easy task for any thoracic surgeon familiar with thoracoscopic procedures.
Then why is there such a wide-spread variability regarding the incidence of intra-operative complications and the clinical outcome (desired result vs. undesired sequelae)?
It seems reasonable to focus on technical parameters that may explain this issue, since patient related factors should be neutralized by having included significant numbers of patients in the study.
The following factors regarding the interruption of the sympathetic chain may be crucial when analyzing the topic from a methodological point of view:
Among the large number of publications on thoracic sympathectomy, the majority lack an exact description of these elements.
Why is there such a big discrepancy between the outcome in different individuals (besides patient related factors)?
This makes the outcome to a sort of lottery (to the patient): if the anatomical situation has been advantageous, or if mother nature, in the process of healing, has been forgiving, even too radically or less meticulously carried out procedures may yield satisfactory or, at least, acceptable results.
In 2011, the Society of Thoracic Surgeons (STS) published an Expert Consensus for the Surgical Treatment of Hyperhidrosis, attempting to define “best procedures” and to standardize the nomenclature. Unfortunately, the consensus was based on previous publications, most of them reporting the employed surgical technique too vaguely to allow extracting reliable deductions from the published results. Furthermore, in their conclusions, focus has been put on minimizing hypothetical recurrencies, occurring in almost negligible frequency, instead of reducing the impact of side effects (significant incidence). According to this consensus document, the interruption should be rib-oriented and directed to the top of the aimed-at rib. Most astonishingly, ganglion-oriented sympathectomy is considered unreliable due to the variability of the anatomy and location of the ganglia.
This appears to be really remarkable: the sympathetic chain is the target of action and basis of evaluation of the results of surgery, but the recommendation is to aim at and refer to the underlying scheleton without taking care of the anatomy of the nerve; in other words: do not aim at the organ you are intended to operate, because it may shift up and down, aim instead at a nearby structure that seems anatomically easier to identify and more stable in its location (!). Needless to emphasize that this singular concept introduces and consolidates a system error, reproduced by all surgeons that follow these recommendations, which makes it impossible to determine where on the nerve and to what extent the damage has been carried out.
In addition, no critical analysis has been undertaken regarding the different means used to interrupt the nerve and their physical effect on the tissues.
If the objective of the Expert Panel had been to gain a better understanding of the desired and undesired effects of sympathetic surgery, their recommendations will barely reach the goal. The only result would be to universalize the vagueness of the procedures and reports, because based on hitting the sympathetic chain blindly, with whatever method, without knowing which ganglion is severed and to what extent the ganglion is destroyed. The consequence is that most studies will be relatively useless for gaining better knowledge on the subject.
In addition, there is the lack of standard in reporting side-effects, particularly the incidence and the degree of compensatory sweating, spanning over a wide percentage range in different publications.
In the past 20 years, awareness of side effects has become more wide-spread. Attempts have been proposed to reverse the surgery, repair the chain (reconstruction of the sympathetic chain with different techniques), counteract side-effects with drugs and local treatment. However, a detailed critical scrutiny of the surgical techniques has never been endeavoured, to find an explanation for and, eventually, seek to prevent excessively undesirable results.

|

|

|
When reading published studies, one get the impression that many surgeons are not aware of the real anatomy of the sympathetic trunk and its variability.
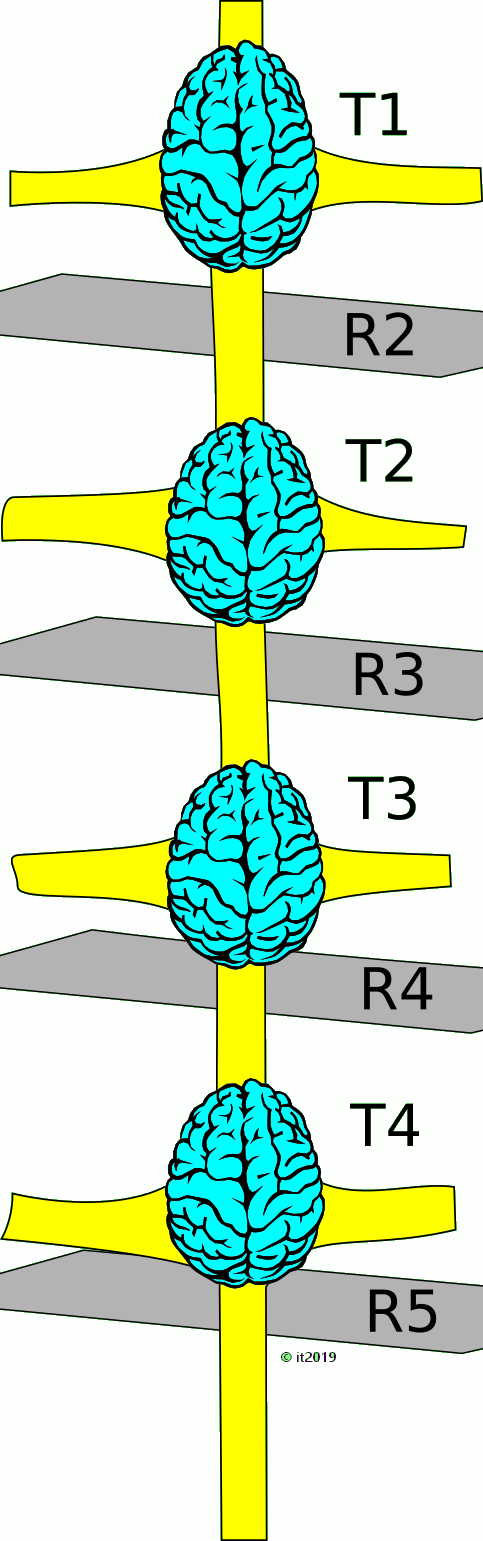
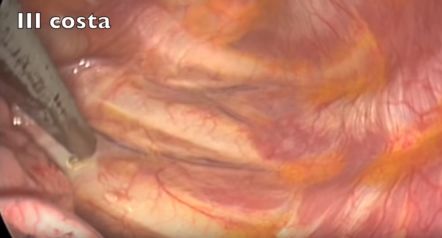
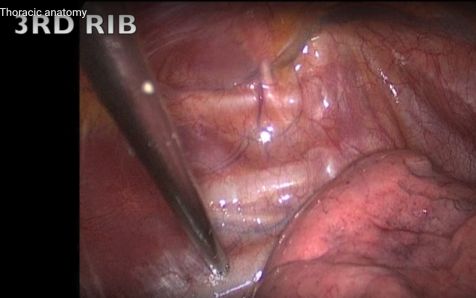
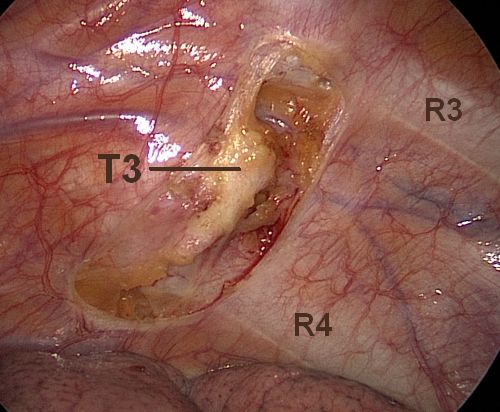
It seems not universally known that a sympathetic ganglion almost always is located in the lower part of the intercostal space, beginning at some distance below the lower edge of the rib carrying the same number, and, more often than not, reaches down to or even covers, partly or completely, the next rib (e.g. the T3 ganglion has no contact with the 3rd rib, but reaches or overlies the 4th rib).
That implies that the widely adopted method to use the ribs as main landmark will interrupt the nerve at a casual level, may fail to target the correct ganglion or sever a ganglion that was not intended to be addressed. The extent of damage to the nerve may be fortuitous and unpredictable, even depending on the technique adopted to interrupt the chain. It may result in partial damage to the ganglion and possible creation of a neurologically unstable ganglion.
| Relationship between the 4th rib and the ganglion T3 at the exit point of the grey ramus communicans, representing roughly the middle of the ganglion (percentage of findings in 121 patients = 242 thoracic cavities) - Study (ISSS Symposium, Vienna 2005). In almost 2/3 of the cases, this connection point is located at or below the 4th rib. In the remainder, around 1/3, the connection was found above the 4th rib, which however does not exclude the lower part of the ganglion reaching or overlapping the rib. | |

|
 Example of T3 ganglion located on and below the 4th rib. Example of T3 ganglion located on and below the 4th rib.
RC: ramus communicans. ICN: intercostal nerve R: rib |
Level misjudgment: Another possible pitfall is the wrong interpretation of the level (wrong numbering of ribs), repeatedly documented in published videos (!) in the net. I am afraid that the examples found in these videos are only the tip of the iceberg and, in reality, misinterpretation of the anatomy is far more frequent.










A considerable number of surgeons are not familiar with the physics of electrocautery, leading to analogous risks, as mentioned in the preceding paragraph, resulting from the uncritical use of this device:
Pure cutting current (continuous unmodulated current >=200V), on the other hand, applied on a minimal surface (needle electrode or tip of L-hook) will cause optimal and concentrated energy delivery to the tissue, resulting in a clean cut with a  sealed cut surface and minimal heat penetration into the underlying tissue. At the point of contact, the tissue cells will boil and literally expload in milliseconds, the vapor creates an immediate raise in tissue impedance (resistance) that prevents further penetration of electrical energy and spreading of heat to deeper layers. This electrocautery technique, along with clipping, is more precise, requires relatively low energy and should, therefore, be preferred over other techniques based on heat delivery, including laser.
sealed cut surface and minimal heat penetration into the underlying tissue. At the point of contact, the tissue cells will boil and literally expload in milliseconds, the vapor creates an immediate raise in tissue impedance (resistance) that prevents further penetration of electrical energy and spreading of heat to deeper layers. This electrocautery technique, along with clipping, is more precise, requires relatively low energy and should, therefore, be preferred over other techniques based on heat delivery, including laser.
The same pattern of continuous unmodulated current below 200V will not reach sufficient tissue temperature to vaporize the intracellular water, but leads to Soft Coagulation that spreads gradually through the tissue, without carbonizing it. This technique is the preferred method to stop bleeding in a pinpoint fashion, but should not be used to interrupt the nerve because it is difficult to determine with sufficient precision the extent of thermal damage along the nerve.

Standard Coagulation and Blend mode (cutting + coagulating) requires higher peak voltage settings compared to pure cutting current and has the property to penetrate deeply into the tissue and spread heat uncontrollably along the nerve. Applied long enough, it will carbonize the tissue. Superfluous to mention that its inaccurate use may cause partial thermal damage to the adjacent ganglia or to contiguous structures (intercostal nerve, costovertebral joint etc.), if not employed with extreme caution. Even more dangerous is the use of Fulguration mode in such sensitive environment as the thoracic cavity, characterized by voltage settings as high as to create sparks to reach the tissue even without direct contact. Some surgeons have the (hazardous) habit to apply cut/coag-energy on the electrode while pushing it against the targeted structure (e.g. a nerve), instead of grabbing and lifting it away from the underlying tissue before switching on the current. This technique makes it difficult to limit the depth of mechanical and thermal damage. On the other hand, when pulling the nerve (e.g. with the hook electrode) and applying too low energy, heat will spread rapidly along the nerve and cause more extended necrosis than intended, without or before dividing it.

Frequency: 200 - 3300 kHz (no neurostimulation occurs above 100 kHz)
Nerve tissue is destructed at temperatures at or around 70°C and remains intact at or below 40°C. Unstable nerve tissue due to permanent permeabilization of the axon or cell membrane, an issue not yet addressed in publications dealing with sympathetic surgery, may develop in the layer between necrotic and still healthy tissue, giving rise to chaotic depolarization of nerve fibers and uncontrolled discharge of neurons if the segment includes a ganglion, thus producing pathological nerve signals.

In the early days of ETS (Kux 1977 and later in the 80-ies Claes and Drott), there was a tendency to proceed radically enough in order to guarantee total dryness with least possible risk for recurrence. Consequence of this philosophy was the interruption of the sympathetic chain on different levels, originally severing the sympathetic trunk over the 2nd, 3rd and 4th rib (later in the 90ies reduced to 2nd and 3rd), employing high intensity electrocautery, without identifying the exact location of the ganglia.
Interestingly, this technique is still widely in use, presumably because many surgeons, beginning to perform ETS, rely on the original description of the technique, having in the meanwhile been adopted on thousands of patients.
A turning point has been the report by CC Lin who, besides having introduced the clamping method, postulated the efficacy of the T4 approach for palmar hyperhidrosis, which later was included into the Lin-Telaranta-classification.
Personally, the author was not able to reproduce the excellent results of ETS T4 reported by Lin. In a series of 16 patients, in whom the T4 ganglion was dissected free, isolated and completely destroyed, the side-effects were admittedly greatly reduced, but the desired effect was not reliable: in some patients, the result was asymmetrical, in some the reduction of sweating was insufficient and others experienced a relaps within months. Over half of the patients required repeat surgery, inducing me to climb a step higher and target the T3 ganglion ever since, focussing exclusively on the ganglion, not on the rib.
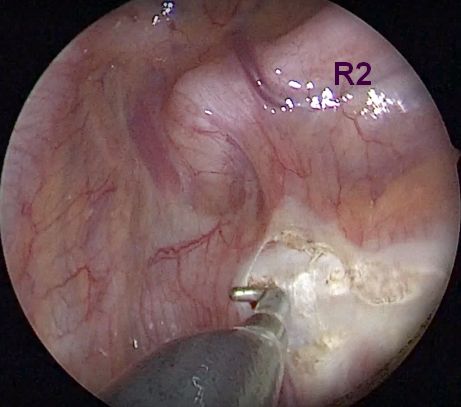
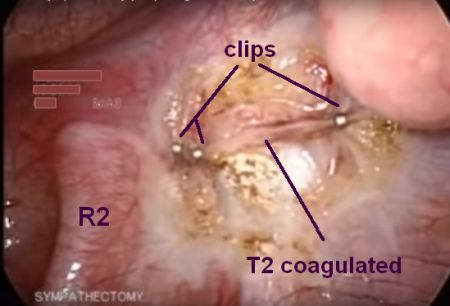
The explanation for this incongruency became clear when observing Lin performing the surgery at the bi-annual symposium on sympathetic surgery in Tampere, Finland, in 2001. He used to place 1 clip above and 1 clip below the 4th rib (Fig.). From an anatomical point of view, the T3 ganglion was compressed by the upper clip, while the T4 ganglion remained completely unharmed by the procedure. This supported the view that isolating and/or destroying the T3 ganglion would be the best compromise to obtain a good and enduring result in patients with hyperhidrosis of the upper extremity, while reducing side-effects to a tollerable minimum. Neutralizing the ganglion was carried out by interrupting the interganglionic segments above and below the ganglion and the grey ramus communicans, using either clean cutting diathermy (with final or careful soft coagulation of the ganglion itself) or by applying clips without destroying the ganglion. No significant difference regarding the result was noted between the two methods.
Surprisingly, apart from improved side effects, the rate of clinically significant recurrence of palmar sweating dropped to almost nil, compared to the T2 method adopted in the preceding decade.
Similarly, the T3 method according to the Lin-Telaranta-classification for facial hyperhidrosis and, especially, facial blushing, did not deliver reliable results when excluding the T3 ganglion alone. Applying the clip or cutting above the 3rd rib may, however, damage the T2 ganglion sufficiently to get the desired effect. Better, though, the interruption carried out above the upper end of the T2 ganglion (corresponding almost always to the lower edge of the 2nd rib) will block all signals directed headwards without damaging the T2 ganglion. However, this will also interrupt a significant number of afferent fibers, deputed to backfeed information about peripheral skin temperature. When the face starts sweating, these fibers report back that skin temperature is beginning to decrease, thus reducing the efferent response to the sweat glands. Disrupting this mechanism may result in more significant reactive sweating, particularly in individuals with an improperly working “thermostat” (like many of those suffering from facial hyperhidrosis at relatively low outside temperatures or after slight physical activity).
Cutting/coagulating/lasering the trunk mid over the anterior surface or on top of the 2nd rib is never required and carries an avoidable risk of damaging the stellate ganglion, particularly in case of a lower than average location of the ganglion (in around 0.3% of cases it covers the anterior face of the rib, partially or completely, resulting inevitably in a Horner's syndrome).

| + |
|
| – |
|

| + |
|
| – |
|
| + | none |
| – |
|
| + |
|
| – |
|
Far too often and by too many used to obtain broad coagulation. High settings will have a cutting effect and prolonged energy delivery will carbonize the tissues. This mode should not have any place in surgery on the sympathetic chain, due to its deep and uncontrollably necrotizing effect on nerve and surrounding structures.

Even more dangerous and destructive than standard coagulation. Off limits for ETS.

Commonly used when employing ultrathin needle-scope (3 mm) and trocars (2-3 mm) that do not accomodate hook dissectors, but only tiny ball-tip electrodes. One may question the cosmetic advantage of reducing the scar in the skin by 2-3 mm, while risking larger damage inside along the chain...
Similar thermal effect as blend or fulgurating mode electrocautery with difficult to judge and limit the extent and depth of heat damage.
| + | delivers clean cut edges with minimal tissue necrosis |
| – | lack of seal on cut edge may lead to neuroma formation |

| + | delivers clean cut edges with minimal tissue necrosis and good seal, similar to plain cutting current |
| – |
|
Excising/destroying part of the sympathetic chain requires extreme attention to detail, in order to avoid an unnecessary long segment and keep traumatization of surrounding and attached structures to a minimum.
The result from resection/destruction of a segment may vary widely depending on
Ganglionectomy of the T3 ganglion (ganglion-oriented, not rib-oriented!) has shown to be effective in close to 100% of patients with palmar or palmo-axillary hyperhidrosis. If damage to the T2 ganglion is avoided, the procedure results in mild or limited side effects and appears to be the best compromise between desired long-term outcome and undesired sequelae.
Any sympathectomy including more than one ganglion is almost never required.
Facial hyperhidrosis and facial blushing should never be treated with resection of any kind.
There is a huge variety of methods that run under the same umbrella term "ETS". The following section lists the most common among the large array of methods employed by different surgeons to carry out ETS. The great number of possible combinations of methods makes it difficult to give an all-comprehensive listing. Only a few of these procedures follow sound neurosurgical and neurophysiological principles (green), others are acceptable but not optimum (yellow). Most procedures cause, however, more damage than necessary and should be avoided, even if they are still widly in use.
The surgeon uses the 2nd rib as landmark to interrupt the nerve. The rib is vertically crossed by the nerve fibers that connect the T1 (stellate ganglion) with the T2 ganglion. The position of the T1 ganglion may vary and could be very close to or, exceptionally, even overly the rib, exposing it to risk for damage (Horner's syndrome).




 Clip at top and bottom edge of 2nd rib + fulguration of pleura and periosteum lateral to the chain (rationale of such traumatization?). Clips applied in an unstable way perpendicular to rib and pointing at lung. Furthermore, as declared in the video, this questionable procedure is performed for treatment of palmar hyperhidrosis (!).
Clip at top and bottom edge of 2nd rib + fulguration of pleura and periosteum lateral to the chain (rationale of such traumatization?). Clips applied in an unstable way perpendicular to rib and pointing at lung. Furthermore, as declared in the video, this questionable procedure is performed for treatment of palmar hyperhidrosis (!).








In the literature, the "T3 procedure" has become the most frequently mentioned method to treat palmar hyperhidrosis in the past 15 years. Most of the described methods refer to the 3rd rib and do not even come close to the T3 ganglion. The surgeon uses the 3rd rib as landmark to interrupt the nerve. The rib is vertically crossed by the nerve fibers that connect the T2 with the T3 ganglion. The lower segment of the T2 ganglion lies often very close to or covers partially the rib.


This will block the chain between ganglion T2 and T3 (interganglionic ESB).







 )
)





The surgeon uses the 4th rib as landmark to interrupt the nerve. The T3 ganglion in most cases touches the top margin of the rib or covers the rib partly or totally. The T4 ganglion has no contact with the 4th rib: its upper end begins at some distance from the 4th rib's lower margin.














Usually performed by severing the sympathetic trunk with electrocautery where it crosses the 2nd and 3rd rib (more or less extended on anterior face of rib).

The cut/coag sympathicotomy R2-R3 (generally, but misleadingly termed ETS T2-T3) was a common surgical method in the 1990-ies and is still widely in use, despite having (or should having) been superseeded by more recent surgical technique.
The potential risks regarding the stellate ganglion during interruption at the 2nd rib level are mentioned above (ETS T2). The procedure leaves the T2 ganglion more or less harmed. Complete neutralization of the T2 ganglion is only guaranteed if the intervening segment stretching over the intercostal space is additionally coagulated or resected. Otherwise, the injury to the T2 ganglion may result partial, possibly leading to a potential hot spot due to chaotic depolarization of unstable nerve tissue membranes. The T3 ganglion is rarely involved (only when using massive coagulation energy over the 3rd rib, the distally located T3 ganglion may suffer marginal damage).
From a therapeutical point of view, there is no rationale today to persevere with this approach. On the contrary, it only may contribute to increase the risk for complications and side-effects.




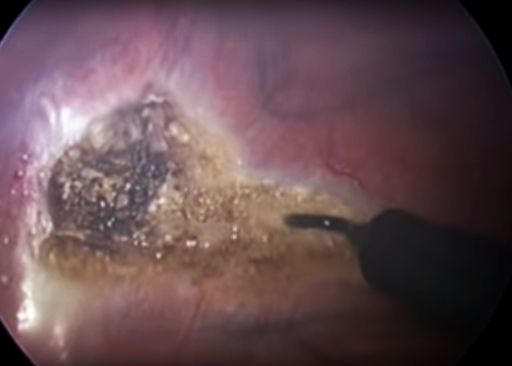
This triple division of the sympathetic trunk is generally also performed using electrocautery, where the chain crosses the 2nd, 3rd and 4th rib, using varying degrees of thermal energy on the ventral surface of the ribs.

The result is usually partial injury to the T2 and heavy injury to the T3 ganglion, unless the intercostal segments of the sympathetic chain, carrying the two ganglia, are additionally coagulated or in toto excised.
The cut/coag sympathicotomy R2-R4 (generally, but misleadingly termed ETS T2-T4) was the most common surgical method in the late 1980-ies and at the beginning of the 1990-ies. There is evidence (e.g. Youtube videos) that it is still in use in a series of thoracic surgery units around the globe, presumably because of many surgeons basing their procedures on publications dating back to the initial pioneering era.
The risks are the sum of risks mentioned above for the single level rib-oriented procedures.
Today, there is no indicaton for exposing the patient to such traumatic practice and should be definitively abandoned.












Generally performed by severing the sympathetic trunk with electrocautery where it crosses the 3rd and 4th rib, delivering varying levels of thermal energy to the anterior face of the ribs.

The result on the sympathetic trunk is a partial, subtotal or complete destruction of ganglion T3, due to proceeding on the 4th (!) rib, since the T3 ganglion often extends down to or over the 4th rib. Severing the nerve at the 3rd rib level will, in the best of cases, divide the interganglionic segment T2-T3; more often, the anatomical situation is less favorable and the T2 ganglion could suffer damage.
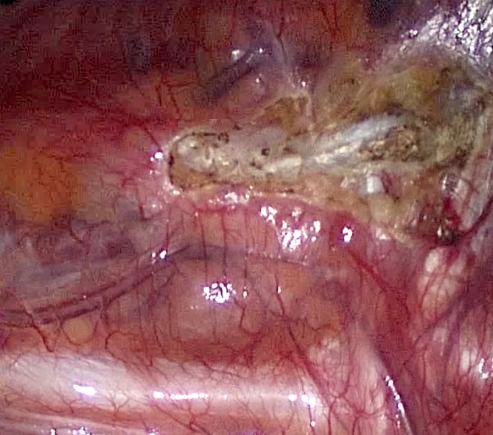
Video  showing bilateral sympathicotomy on both R3 and R4 levels with harmonic scalpel. Since ganglion boundaries are not respected, ganglion T3 is partially injured (maybe also T2).
showing bilateral sympathicotomy on both R3 and R4 levels with harmonic scalpel. Since ganglion boundaries are not respected, ganglion T3 is partially injured (maybe also T2).
Excising the intervening segment will generally encompass the T3 ganglion. Exceptionally, in case of low-sitting T3 ganglion, only the upper portion of the ganglion will be involved. The T4 ganglion remains practically always untouched. Exact location and mode of division (scissors or type/energy of current), as well as coagulation of bleeding vessels determine possible extended damage to neighboring ganglia (T2, T4) and thermal injury to intercostal nerves.
As any rib-oriented procedure, the target (i.e. the sympathetic chain) is hit fortuitously, disregarding the anatomical boundaries of ganglia and interganglionic segments.
Including the R5 level is supposed to increase the chance to treat axillary hyperhidrosis.

Anatomically, it would cause variable damage to the T4 ganglion (without involving the T5 ganglion).
Controlled evidence is lacking that would prove that resecting or coagulating the T4 ganglion only, or in addtion to the T3 ganglion, would be more effective to suppress axillary hyperhidrosis than neutralizing the T3 ganglion alone.
Experience has shown that excluding the T3 ganglion will treat not only palmar, but also coexisting axillary hyperhidrosis with good and enduring effect in most cases.
As always when applying heat energy on - and particularly on top of - the 3rd rib, the T2 ganglion is in likely to be harmed, possibly leading to serious side effects.






There are various methods to block, destroy or excise the T2 ganglion, but damage or exclusion of the T2 ganglion is almost never required and shoud be avoided. A minority of patients may suffer potentially severe thermoregulatory or cardiovascular side-effects (see conclusions). Only the interganglionic segment between T1 and T2 should be interrupted, taking care to leave both ganglia unharmed. To keep a safe distance to both ganglia, the interruption would have to be executed immediately underneath the lower edge of the 2nd rib. Should reconstruction in case of unbearable side-effects ever be required and attempted, a chance of recovery of the nerve function would only be possible if the interruption had been carried out in this precise location and without damage to the ganglia.
Facial blushing requires blocking the rostrally directed nervous signals exiting T2, which can best be achieved by interrupting the interganglionic segment between T2 and T1 (stellate ganglion), keeping a safe distance to T1. As mentioned, the interruption is best carried out at the lower edge of the 2nd rib, carrying out one single clean cut or, better, applying one single clip).

The same procedure will reliably control facial hyperhidrosis, but with a higher risk for postoperative compensatory hyperhidrosis. Patients with this type of HH are often highly thermo-sensitive, their central thermostat being “programmed” to react more intensely to increasing outside or body temperature than the average person. Interrupting the afferent sensory fibers running in the sympathetic chain may disrupt the required sensory feedback that fine-tunes the response of the thermoregulatory system. The result could conceivably be an uncontrolled massive outflow of efferent signals directed to the sweat glands of the trunk. Therefore, the patient selection has to be very accurate and the preoperative information to the patient should focus on this elevated risk. The clamping method should be preferred. Interruption of the interganglionic segment T2-T3 (one level lower applying one single clip at lower margin of 3rd rib) may be an alternative procedure, obtaining reduced facial sweating in some. Side-effects are usually less, but the desired effect is not reliably predictable and some patients may require redo surgery (clamping one level higher).
Neutralizing the T3 ganglion will effectively cure palmar hyperhidrosis with excellent long-term result and has shown to yield the best compromise between desired result and undesirable side-effects. It is also highly effective in reducing associated axillary hyperhidrosis.
The ganglion is dissected free and exactly identified (in some cases, the ganglion can even extend beyond the lower edge of the 4th rib). Its upper end is always located below the lower edge of the 3rd rib (!). Interruption should be carried out at the interganglionic level, at the lower margin of the rib, not across any part of the ganglion. It is not clear, whether destroying the ganglion will add to the longterm efficacy.

1 clip on lower margin of 3rd rib, 1 clip on lower margin of 4th rib (with or without additional clip on grey ramus communicans - grc) . The ganglion itself will remain intact and continue to be viable, but exiting connections will be blocked.





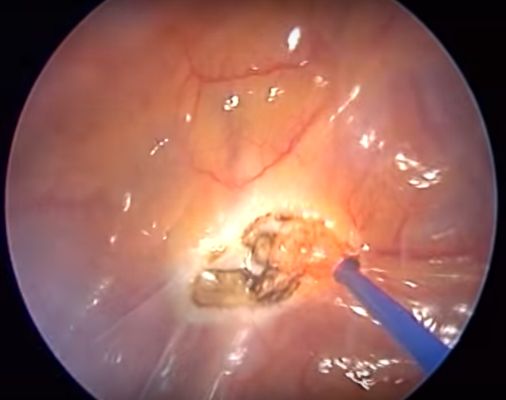
Ganglion is isolated by clean division (pure cutting current) at lower edge of 3rd rib and lower edge of 4th rib, careful (=soft) coagulation of the ganglion while lifting the ganglion from the underlying structures and keeping continuous awareness of the distribution of current density and heat development. This procedure is comparable to resection of the ganglion, but can be accomplished with a 2-port approach. Excellent method for palmar hyperhidrosis to achieve reliable long-term results with limited side-effects.

Any other technique (use of blend current, division in other locations, fulguration, coagulation of ganglion while pressing against underlying structures, etc.) implies a significant risk of damaging adjacent ganglia and/or underlying structures (intercostal nerve, costovertebral joint, etc.).

Clean division (plain electro-cut or scissors with application of clips to seal the cut-edge) at lower edge of 3rd rib and lower edge of 4th rib, excision of the ganglion, if necessary careful (soft) coagulation of bleeders without damaging adjacent or underlying structures.
There are several variants to this technique (no seal, heavy coagulation due to bleeding, division in the middle or on top of the rib, etc) that carry always a risk for causing collateral damage and, consequently, post-operative discomfort and long-term side-effects.


This term implies blockade, destruction or removal of both ganglia T2 and T3.

As a rule, there is no rationale for eliminating both ganglia. It only risks adding or increasing the intensity of side-effects, without improving the desired outcome.
As with other variants of ETS, there are different surgical techniques in use to accomplish the task.
Severing the sympathetic chain above ganglion T2 and below ganglion T3 is followed by either coagulation or resection of the intervening segment containing the two ganglia.
Besides the superfluous destruction/excision of the T2 ganglion, collateral damage may occur if coagulation is used generously to stop bleeders or fulgurate the ganglia.
An odd variant of this principle consists in severing the rami communicantes of the ganglia T2 and T3, followed by blocking the chain above the T2 ganglion and at the level of the T3 ganglion, without resecting the segment.


Destruction or removal of both ganglia T3 and T4.

Sometimes used in patients with combined palmar and axillary hyperhidrosis. Generally, after a complete destruction/excision of the T3 ganglion, also sweating in the armpit ceases or is reduced to normal level. Including the T4 ganglion is considered by some surgeons to reduce the recurrence rate of axillary sweating.
As with other variants of ETS, there are different surgical techniques in use to accomplish the task.
Severing the sympathetic chain above ganglion T3 and below ganglion T4 is followed by either coagulation or resection of the intervening segment containing the two ganglia.
When resecting, collateral damage may occur if coagulation is used generously to stop bleeders or fulgurate the ganglia.

Neutralization of the T4 ganglion alone will, if carried out cleanly, regardless of technique (as described above -> ETS T3 ganglion-oriented), yields inconsistent results when used to treat palmar hyperhidrosis.
The author has no experience in treating isolated axillary hyperhidrosis with this method.
“Dirty” cuts on the 4th rib may damage the T3 ganglion sufficiently to “improve” the result, but such procedure has to be classified as rib-oriented R4, not as ganglion-oriented T4 procedure.
Resections imply removal of a section of the sympathetic chain.
Crucial elements of a resection are the following parameters:
Since the division and dissection of the nerve can be carried out by any of the above mentioned methods, the least traumatizing one should be chosen, keeping spread of thermal damage to a minimum. Anatomical boundaries of the chain should be respected, avoiding partial damage to a ganglion, including cutting through a ganglion.
Facial hyperhidrosis and facial blushing can be treated by one single interruption (cut or, preferably, clip). Ganglion resection is never indicated nor required.
Palmar or palmo-axillary hyperhidrosis is best dealt with by neutralizing the ganglion T3. This can be accomplished by resection or by careful coagulation of the ganglion, after detaching it at either end, and leaving it in place. Alternatively, the T3 ganglion can be efficiently isolated by applying titanium clips above, below and on the grey ramus communicans.
Resection of the T2 ganglion or extended excisions, involving multiple ganglia (like in the following examples), are almost never required and should be avoided.
T2-T4 (cutting and blend mode electrocautery)

Video
T3-T5 (harmonic scalpel)

Video 
T2-T3 (blend mode electrocautery)

Video 
T2-T6 (left), T3-T7 (right) - Robot assisted sympathectomy (blend mode electrocautery): a questionable method.
Right image: heat damage to the lung (lower left). The bad habit to use the grasping forceps for coagulation and, indeed, to cut(as shown in the video!), may result in unintentional heat injury to adjacent structures if the surgeon does not keep the unisolated surfaces of the instrument under control.
Video 
Attention! When dividing the nerve with clean cutting current, broad tissue contact with electrode will disperse energy and result in soft coagulation instead of a cut:


ETS is an extremely valuable method to treat palmar hyperhidrosis, but it has to be done correctly, at the correct level, with precision, and using the least traumatic method available. The problem with ETS is not the principle itself, it is the way it is carried out. And unfortunately, with most of the methods described, the patient must rely on his/her luck not to end up with heavy undesired side-effects.
ESB (block with single clip) may also be a good solution for patients with debilitating facial ailments which do not respond to conventional therapy. However, the recurrence rate is higher for facial blushing, and, for facial hyperhidrosis, patient selection has to be particularly strict, because of the significantly higher risk for compensatory/reactive hyperhidrosis in this latter category of patients. Reversal (removal of the clip) will only lead to reduction of compensatory sweating if the nerve had not been completely crushed by the clip.
Technical hints and summary